In healthcare, Nursing Report Sheets have long been a staple for passing critical patient information between shifts. When used thoughtfully, these sheets support safer care by preserving continuity, clarifying responsibilities, and highlighting changes in a patient’s condition. This article examines common myths about Nursing Report Sheets and explains how they can enhance safety when paired with good clinical judgment and robust handoff processes.
Key Points
- Nursing Report Sheets are a communication tool, not a substitute for direct patient assessment or ongoing monitoring.
- Standardized formats help minimize omissions and reduce misinterpretation during handoffs.
- Timely updates and clear ownership of information are essential for safer care.
- Privacy and accuracy require thoughtful design and ongoing team training.
- Digital options can augment paper sheets but must be implemented with careful attention to workflow and privacy.
What Nursing Report Sheets are and aren’t
Nursing Report Sheets are structured summaries used during shift changes to convey the patient’s current status, recent changes, medications, allergies, and priorities for the next care team. While they are powerful tools for ensuring continuity, they are not a substitute for direct patient assessment, ongoing observation, or clinical reasoning. Misconceptions—such as viewing sheets as a complete, immutable medical record or as a catch‑all handoff—undermine safety. In reality, report sheets are one piece of a larger handoff system that includes bedside communication, active clinical monitoring, and careful documentation in the chart.
How Nursing Report Sheets contribute to safer care
When used well, Nursing Report Sheets reduce information gaps between shifts and help the incoming team identify high‑risk issues, planned tests, and pending decisions. They improve accountability by clearly marking who is responsible for what and what actions are imminent. In addition, standardized sheets support consistency across providers and units, which lowers the chance of critical details being overlooked during busy periods. The result is a smoother transfer of care that protects patients from avoidable errors and delays.
Debunking myths with practical guidance
Myths about Nursing Report Sheets often stem from a tension between speed and accuracy or from skepticism about paper versus digital tools. Here are practical clarifications that address common concerns:
Myth 1: They replace bedside assessment. Reality: They summarize and communicate current observations, not replace clinical judgment or ongoing patient evaluation.
Myth 2: More information is always better. Reality: Relevance and clarity matter. Concise, prioritized details prevent overload and misinterpretation.
Myth 3: Paper sheets are outdated. Reality: Paper can be highly effective when designed to fit workflow; digital systems should augment—not disrupt—handoffs.
Myth 4: Handoffs are a one-way transfer. Reality: They should prompt questions, verification, and collaborative planning between shifts.
Myth 5: Privacy concerns lock out useful information. Reality: Safeguards and role-based access can protect privacy while preserving essential clinical details.
Best practices for effective use of Nursing Report Sheets
Adopting evidence‑informed practices helps ensure that Nursing Report Sheets truly support safer care. Consider the following guidelines:
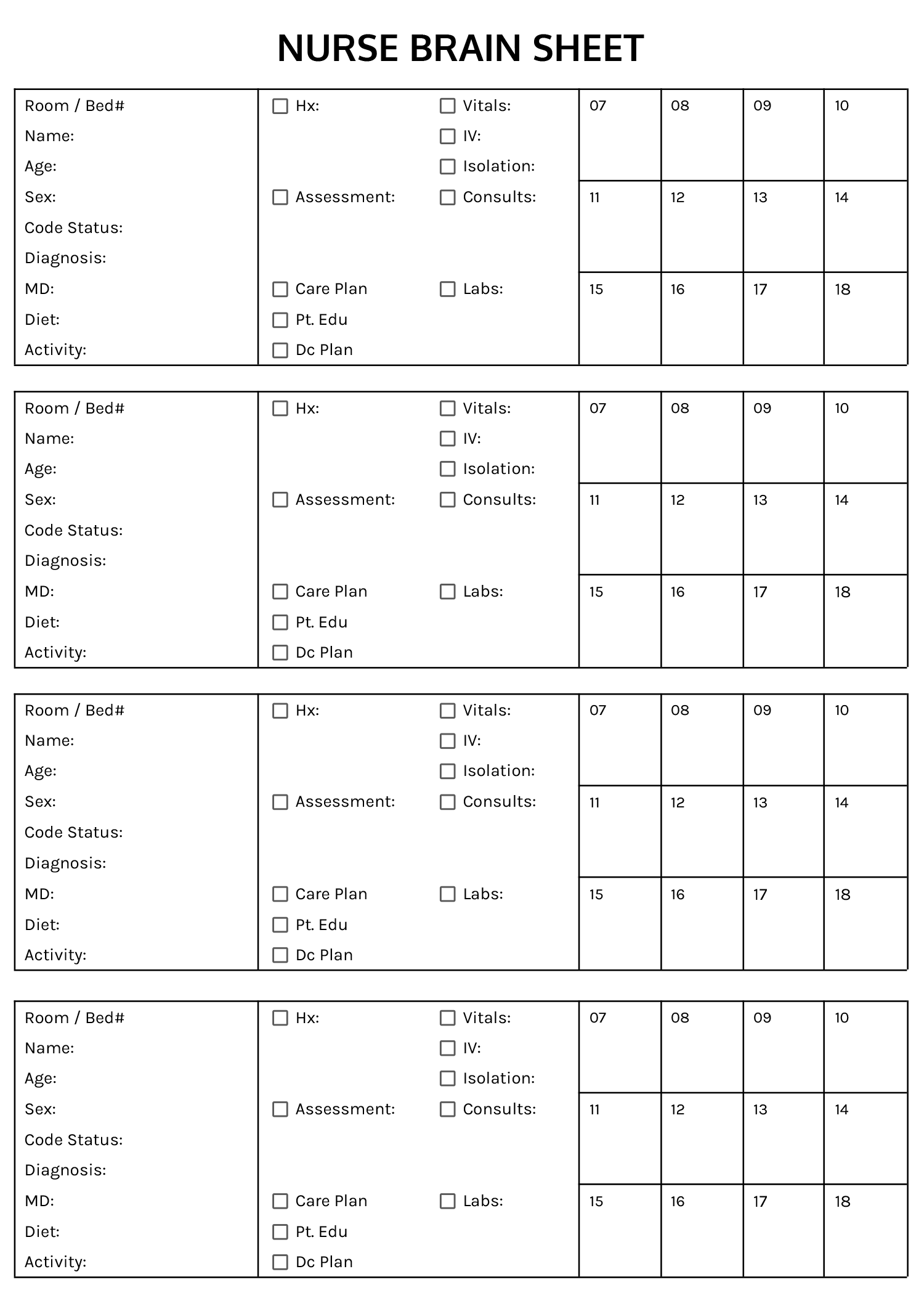
- Adopt a standardized template that highlights patient name, diagnosis, current meds, allergies, alerts, recent changes, and pending tasks.
- Include a brief “no‑surprises” section that flags critical issues requiring immediate attention.
- Use concise language and avoid duplicating chart notes; align sheet content with the electronic health record where possible.
- Train staff regularly on handoff communication skills, including check-backs and verification of critical data.
- Respect privacy by limiting sensitive details to appropriate team members and using secure channels for information sharing.
Implementing for safer care: practical steps
To turn the theory into safer practice, teams can pilot improvements in small steps. Start with a quick audit of current handoffs to identify missing data, ambiguities, or repetitive entries. Gather frontline feedback on template usability and adapt the format to fit the unit’s workflow. Pair any transition to digital systems with training and change‑management efforts to preserve the practical benefits of clear, timely information transfer.
What exactly qualifies as a Nursing Report Sheet?
+A Nursing Report Sheet is a concise, structured summary used during shift changes to communicate the patient’s status, plan, and any urgent concerns. It should cover essential details such as diagnosis, allergies, current treatments, pending tasks, and safety alerts, while avoiding unnecessary information that could slow handoffs.
Are Nursing Report Sheets obsolete in the digital era?
+No. The core idea of a reliable handoff remains critical. Digital tools can enhance efficiency and accessibility, but they must be designed to support clinicians without creating new burdens or privacy risks. A well‑integrated system that complements paper sheets can improve accuracy and timeliness.
How can nurses ensure accuracy during handoffs?
+Use standardized checklists, verify critical values with the incoming team, summarize changes since the last handoff, and encourage active questions. Regular training on communication skills and routine audits help sustain accuracy over time.
What safeguards protect patient privacy on handoffs?
+Limit access to sensitive information to authorized staff, anonymize data when possible, and use secure channels for sharing handoff details. Institutional policies and periodic privacy training reinforce safe practices.
How do we measure the impact of Nursing Report Sheets on safety?
+Track metrics such as handoff completion rate, time to critical alerts, incident reports related to communication gaps, and staff satisfaction with the handoff process. Use these data to drive iterative improvements and share successes with the team.